Experts answer 7 frequently asked questions about epilepsy.
More than 2 million people in the United States have some form of epilepsy, a group of related disorders marked by recurrent seizures. WebMD asked epilepsy experts your most frequently asked questions.
How do people develop epilepsy?
In most cases — about seven in 10 people — the cause of epilepsy is unknown. In other cases, epilepsy can have a symptomatic cause, such as birth injuries, head injuries, and infectious diseases including meningitis and encephalitis. It can also be caused by genetic conditions and stroke.
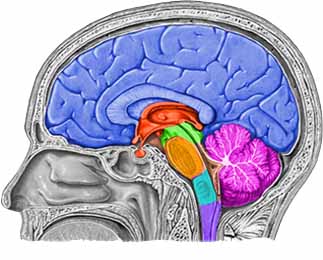
“Whatever the cause, epilepsy causes too many nerve cells to fire in the brain at the same time,” says Donald Olson, MD, director of the Epilepsy Program at Lucile Packard Children’s Hospital at Stanford University Medical Center. “Depending on which part of the brain the cells are firing in, the symptoms could vary from a strange feeling, to one side of the body jerking, to a whole-body convulsion.”
How is epilepsy diagnosed?
A doctor will start by taking a medical history, followed by a physical and neurological examination of muscle strength, reflexes, eyesight, hearing, and ability to detect various sensations. Other tests include an electroencephalogram (EEG) test, which measures electrical impulses in the brain; imaging studies of the brain, often with magnetic resonance imaging (MRI); and blood tests to measure red and white blood cell counts, blood sugar, blood calcium and electrolyte levels; and to evaluate liver and kidney function.
What are the types of seizures?
Seizures are divided into two broad categories: partial and generalized.
Partial seizures affect only a specific part of the brain and are further grouped into two types: In simple partial seizures, a person may have jerking movement and abnormal sensations, such as extreme emotion or changes in taste, depending on what part of the brain the seizure affects. In complex partial seizures, a person loses awareness and may have unconscious movements such as lip smacking and fidgeting. Partial seizures that spread and become generalized are called partial seizures secondarily generalized.
Generalized seizures affect the entire brain from the beginning of the seizure and are broken down into several types: In generalized tonic-clonic seizures, the entire body stiffens and jerks and a person loses consciousness. This is also known as a grand mal seizure. Myoclonic seizures are lightning jerks of the muscle, usually on both sides of the body. In absence seizures, a person loses awareness and has a blank stare, as if he or she is looking through you. This is also known as a petit mal seizure. Atonic seizures cause the body to lose muscle tone with no warning and fall over.
What do I do if my friend has a seizure?
“It’s the generalized tonic-clonic seizure that requires the most action,” says Jacqueline French, MD, a professor of neurology at New York University Comprehensive Epilepsy Center and a fellow with the American Academy of Neurology.
What do I do if my friend has a seizure? continued…
First, gently bring the person to the ground and put something under the head so he or she doesn’t hit the floor, French explains. Then turn the person over on the left side — a better position for easier breathing and improved circulation. Turn him or her head slightly down so saliva won’t go into the lungs — and absolutely do not put anything in the person’s mouth. The seizure should end in one or two minutes, maybe even less.
When the person regains consciousness, he or she will be confused, so stay with the person until he or she is back to the person’s normal self. It’s a good idea for those with epilepsy to wear a medical bracelet. If he or she has a seizure and no one is around, the bracelet will tell others what’s happening so they can respond appropriately.
Can a seizure be life-threatening?
Yes, but very rarely. “Status epilepticus is when a seizure lasts longer than a few minutes, which can lead to brain injury and even death,” says French. So, if a seizure hits the three-minute mark, call 911 immediately.
Looking at seizures in another way, they can be life-threatening, especially for children who are not well supervised in certain situations. For instance, never leave a child who has had a seizure alone in the bathtub, explains Olson.
How is epilepsy treated?
The most common way to treat epilepsy is with medication. Specific drugs are prescribed depending on the type of epilepsy or seizure a person has. When medication doesn’t work, surgery is another treatment option. In some cases, a surgeon can remove the area of the brain producing seizures or can interrupt the nerve pathways that signal seizures. For children, a very strict meal plan called the ketogenic diet may reduce seizures.
If a patient doesn’t respond to medication and surgery is not an option, vagus nerve stimulation can help prevent seizures. It works through a battery implant in the chest that delivers small pulses of electrical energy into the brain via the vagus nerve in the neck. The downside: It doesn’t work for everyone, and it is not approved by the FDA for kids younger than age 12.
Any new treatments on the horizon?
“We have a lot of hope that some of the brain-stimulation technologies currently in development will bear fruit,” says Olson. The goal of brain stimulation is to detect and interrupt seizures before they begin, through an implanted device in the brain. New medications are also in clinical trials, such as nasal sprays with antiseizure drugs that could be used immediately when a seizure starts to help stop its progression.
Originally published in the March/April 2008 issue of WebMD the Magazine.
More
In the current wars in Iraq and Afghanistan the “signature wound” is traumatic brain injury (TBI), of which epilepsy is a common long-term consequence. Those who suffer severe head traumas face up to a 50 percent chance of developing post-traumatic epilepsy, and frequently, this chronic condition does not respond to available treatments, imposing significant ill effects on rehabilitation and quality of life. The civilian population is also at risk; TBI accounts for 5% of epilepsy.
Remarkably little is understood about post-traumatic epilepsy. Although head injury is known to put a patient at high risk for development of chronic seizures in both
civilian and non-civilian populations, there is still a lack of research focused on this area. Post-traumatic seizures can develop at anytime after the injury—from within one week to fifteen years later. At this time, there is no way to prevent or cure post traumatic epilepsy.
Now in its third year, CURE’s program, Prevention of Epilepsy after Traumatic Brain Injury, targets funds to basic and applied research on epilepsy related to traumatic brain injury impacting combat, veteran, and civilian populations in order to better understand the causes of epilepsy following TBI and develop interventions and treatments. This program is in partnership with the United States Army Medical Research and Materiel Command (USAMRMC). The program is financed by the USAMRMC, and administered by CURE.
This program supports investigator-initiated research of relevance to the prevention and treatment of post-traumatic epilepsy, including the cellular, molecular, and systems-level understanding of the underlying pathogenic mechanisms; specific approaches to interdict the development of post-traumatic epilepsy; animal models of post-traumatic epilepsy; and investigations of the impact, natural history and epidemiology of post-traumatic epilepsy.
CURE is embarking on its final year of partnership with the USAMRMC for this program. However, CURE is dedicated to continuing support for research in this critical area. With relatively little investment compared to what it deserves, this targeted program has already produced significant results, including a recent exciting breakthrough from Daniela Kaufer, PhD (University of California, Berkeley) and Alon Friedman, MD, PhD (Ben-Gurion University of the Negev, Israel). Drs. Kaufer and Friedman have discovered that drugs known as TGF-beta blockers prevent epilepsy after brain injury in rats. They found that they could prevent the brain changes leading to epilepsy by treating the animals with a drug that blocks transforming growth factor-beta (TGF-beta) receptors. If the findings are confirmed in humans, the TGF-beta blockers may prevent many cases of epilepsy in accident victims and soldiers serving in Iraq and Afghanistan.
Only with increased public and private funding for post-traumatic epilepsy can researchers continue to explore new areas that will one day lead to prevention and cures for epilepsy.
More